Getting dental care is necessary to maintain overall wellness. Without it, a person may experience a range of dental abnormalities that can lead to heart disease, diabetes, trouble getting pregnant, and other health problems, in addition to affecting their oral health.
However, ordinary health policies rarely cover oral and dental treatment. This is one instance where dental insurance is helpful. Preserving dental health is not the only purpose of this kind of coverage. Furthermore, while dental coverage and regular health insurance policies share many similarities, they also have unique characteristics.
In this article, Insurance Business explains how dental insurance works to help clients choose the plans that best suit their needs and budget. This is a useful tool that insurance providers can give their clients.
What is dental insurance?
Dental insurance is a sort of coverage intended to pay for dental care, as the name suggests. Generally speaking, policyholders must pay premiums to have coverage unless provided to them gratis, as is frequently the case with employer-based plans.
There are three common ways to access dental health policies:
- As part of an insurance coverage for health care
- As a stand-alone policy
- As travelers covered by health insurance policies
How does one apply for dental insurance?
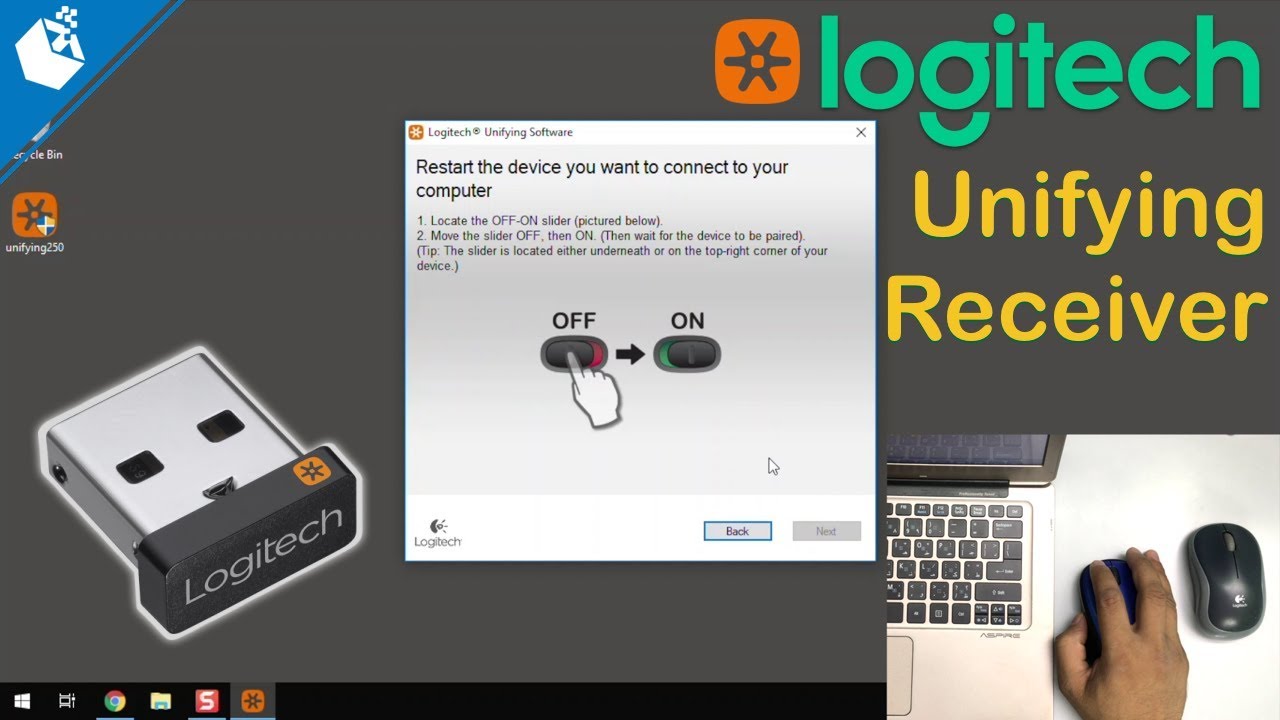
Dental plan members must continue paying payments to keep their coverage, just like with other insurance plans. This can be done every quarter, every six months, every year, or every three months. Company-sponsored plans may be paid for with employee checks.
However, policyholders are also liable for additional out-of-pocket expenses. Plan participants often have to pay the following different costs to receive dental coverage:
Permitted subtraction
This is the maximum amount the policyholder agrees to spend out of pocket before the Insurance company pays the remaining balance. The deductible and the premiums paid are inversely correlated. Stated differently, a lower premium corresponds with a greater deductible and vice versa. One goes up, the other down.
Remember that most preventative care, including routine dental cleanings and exams, does not have a copay.
Participation
Usually referred to as a copay, this phrase describes the amount the policyholder pays out-of-pocket for specific dental procedures, with the insurance company picking up the tab. This may be required at the time of the process.
The table below provides an overview of the numerous out-of-pocket costs the policyholder must pay before dental insurance takes effect.
Coinsurance
When the deductibles are paid in full, the policyholder and the insurer split the cost under a coinsurance arrangement. Most dental insurance plans have a 100/80/50 payment schedule, meaning that the following benefits are implied: 100% coverage for preventative care, 80% coverage for basic services
• A 50% payment refund for major dental repair procedures
Maximum yearly
This represents the most amount the dental insurance plan will cover each year. After this, the policyholder will be responsible for covering the cost of any dental services. The annual coverage maximums often fall between $1,000 and $2,000. Plan holders have access to higher-limit insurance; however, using it will impact rates.
Does dental insurance coverage have any waiting periods?
Most dental insurance plans include waiting periods between six and twelve months before they begin to pay. However, waiting times for major procedures can last up to two years, although wait times for other standard services might be as short as three months. Unlike major and basic operations like crowns and root canals, preventive care typically has no waiting periods.
Insurance companies enforce these waiting periods to discourage customers from getting coverage for future treatments.
What types of dental insurance plans are available?
Like standard health insurance plans, dental policies come in various configurations to meet policyholders’ diverse oral health needs. They are as follows:
Dental Preferred Provider Organization (DPPO)
Under this type of plan, commonly called a PPO, policyholders can pay less for dental care if they receive treatment from providers in the plan’s network. People can also visit dentists, clinics, and other dental care providers only included in the network with a referral for an additional cost.
Dental Health Maintenance Organization (DHMO)
Often, only dentists employed by or under contract with the DHMO are eligible for coverage under this kind of insurance, also called an HMO. These professionals provide coverage at no cost or for a fixed copayment. Nevertheless, professionals outside of the network are not covered by insurance. A policyholder may need to live or work in the service region to qualify for coverage under some plans.
Plans for dental referrals or discounts
Under this insurance, a few participating dentists provide dental services at a reduced cost. The payments are made directly to these providers at the time of treatment.
Plans for fee-for-service or indemnification
Members of this type of coverage, sometimes known as Managed Care on occasion, are free to choose any dentist because it lacks a dental network, unlike DHMOs or DPPOs. Typically, the plan covers a portion of each service, and the patient pays the remaining balance. Additionally, it needs the cheaper fees that other programs provide.
What does dental insurance cover?
Dental insurance policies typically provide three different coverage tiers. They are as follows:
- • Preventive care: Includes fluoride treatments, sealants, X-rays, examinations, and routine dental cleanings.
- • Basic services: Includes root canals (which some insurance considers serious procedures), fillings, simple extractions, emergency treatment for gum and tooth discomfort, root planing, and periodontal scrubbing.
- • Major restorative procedures: These include extraction of impacted teeth, major oral surgery, denture work, bridges, crowns, implants, and anesthesia or sedation.
Some insurance plans cover braces and other orthodontic procedures. Nevertheless, there is a lifetime cap and age limit (usually 18 years old and under).
This summarises the overall amount covered by dental insurance and the extent of each category.
Which procedures are not covered by dental insurance?
Certain insurance includes limitations on the orthodontic procedures—including braces—they will cover. The following are additional services that are typically not covered by a dental insurance policy:
• Cosmetic procedures such as teeth whitening; • Composite or tooth-colored fillings, while amalgam fillings are covered
• Dental care to address pre-existing conditions
Nevertheless, as exclusions vary throughout insurers, policyholders should verify their coverage limitations with their insurers.
What needs to be considered before getting dental insurance?
There may be a great desire to choose the cheapest dental insurance plan based only on price. Industry insiders, however, often point out that “cheaper does not necessarily mean better.” The optimal dental coverage plan should satisfy the policyholder’s oral health needs and financial constraints.